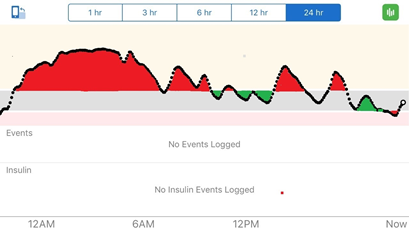
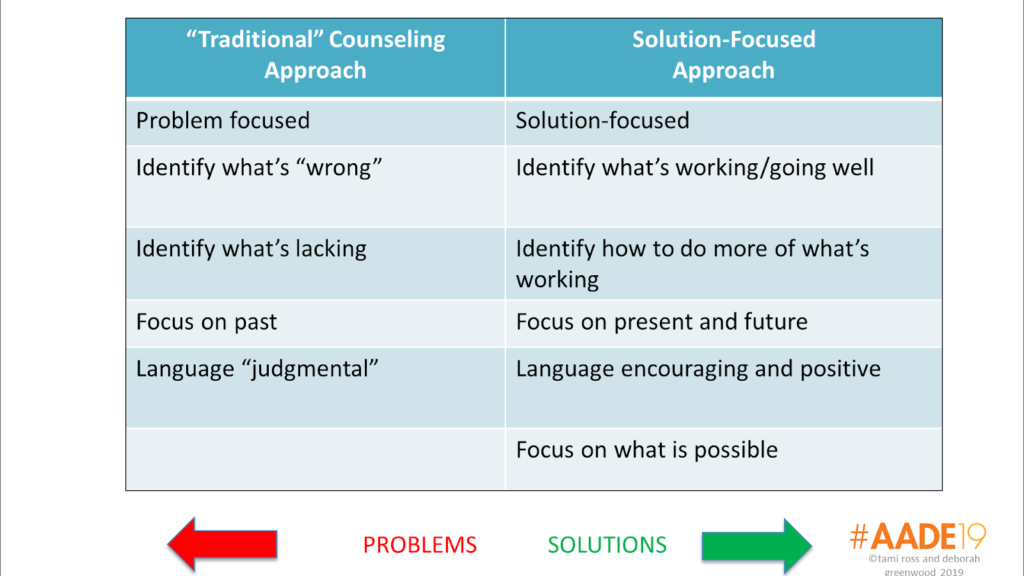
With Thanksgiving celebrations and the holiday season at hand, today we’re sharing 8 tried and true strategies to enjoy the special foods that accompany holiday gatherings without compromising blood glucose. These 8 solution-focused strategies have worked for our clients and we hope are helpful for you.
Strategy 1: Take a healthy dish or treat to share, or a healthier version of a favorite. Maybe it’s something like the caprese kabobs Tami made for an event that you see pictured below. Just a couple of grape tomatoes, fresh basil (or spinach) leaves, and a fresh mozzarella ball speared with a small skewer with a balsamic dressing to drizzle. Offering to bring something healthy can reduce stress by knowing that there’s at least one item to suit personal preferences and needs.(And chances are the host will welcome an addition to the party spread!)
Strategy 2: Share a side dish that incorporates seasonal vegetables. Many of the food traditions associated with Thanksgiving and the winter holidays are laden with carbs and calories. One of our well-loved low carb favorites is roasted vegetables. Whether you choose to roast one type of vegetables (our vote is roasted Brussels sprouts) or a combination of winter vegetables (such as butternut squash, brussels sprouts, radishes (yes radishes!), parsnips, carrots, and red onion) they’re low in carbohydrate, high in flavor, and won’t keep you hanging out in the kitchen. Cut the vegetables into even size pieces/chunks for even cooking, then toss with some olive oil, kosher salt, and black pepper. Roast at 425 degrees in an even layer on a sheet pan until fork tender (about 20-25 minutes). These roasted carrots were delish!
Strategy 3: Try the Two- to Three-Bite Taste Test
Many clients we’ve worked with over the years have shared success keeping their blood glucose in range by sticking with tiny tastings, or 2-3 bites, of foods they may not be sure of exactly what’s in them or foods that are rich in carbohydrate. They can still enjoy the experience without too much worry of sending blood glucose out of range. This is also a great strategy when traveling over the holidays. You can read more about that here.
A patient Tami’s worked with in the past loved cheesecake. Prior to developing diabetes she’d eat an entire giant slice when she dined at her favorite restaurant. Once diabetes entered her life, she still wanted to try to work in cheesecake on occasion, and realized that portion control was important. She agreed to try the two- to three-bite taste test. She reported back that she discovered she really savored the first three bites of her cheesecake, but after that the pleasure decreased. Based on her discovery, she decided to eat just three bites of cheesecake at the meal, count and incorporate the carbohydrate accordingly,
Strategy 4: Make a swap or two. Consider the foods that are often at holiday gatherings and determine where you can make a swap or two for health. One client who is planning ahead shared that she’s planning to swap in broccoli casserole (made with reduced fat ingredients) on her plate in place of mashed potatoes and a corn casserole to reduce carbs.
Strategy 5: Eat off a smaller plate. As we shared in our July 3, 2019 post, when you are ready to sample the celebration spread, if there’s a choice on plate size, go with a smaller plate (maybe the ones that are out for salads or desserts). This strategy helps manage portions, and make those portions appear larger on the full small plate.
Strategy 6: Fill half of your plate with veggies of the non-starchy variety
Aim to fill at least half of the plate with non-starchy veggies (such as veggie salads, green beans, broccoli, roasted vegetables from Strategy 2), one fourth of the plate with lean protein foods (such as a turkey), and one fourth with carbohydrate foods (this is mashed potatoes, stuffing, corn on the cob, or a sweet treat may fit). This simple strategy has brought success for many when navigating picnics and celebrations.
Strategy 7: Cruise by the foods that aren’t worth the carbohydrate or calories. Before filling your plate with a little bit of everything, cruise the buffet or party spread to see what’s available, and then decide which foods you really want, and what portion of each works for you, We encourage asking yourself, “Is it worth the carbohydrate or calories?” If the answer is “no,” then it may be best to pass it by. If the answer is “yes,” then decide what portion fits your carbohydrate budget before adding it to your plate.
Strategy 8: Focus on fellowship and laughter. We believe that laughter is the best medicine, and we try very hard to practice what we preach. Scientists have shown that laughter is a great stress reliever and causes mental relaxation. Laughter can even improve blood pressure, pain, and immunity. Most importantly it strengthens human connections when we laugh together. There is now actually “laughter therapy” defined by the National Cancer Institute as therapy that uses humor to help people cope with medical conditions by relieving pain, stress and improving well-being. Here we are embracing this strategy a few years back on holiday escape!
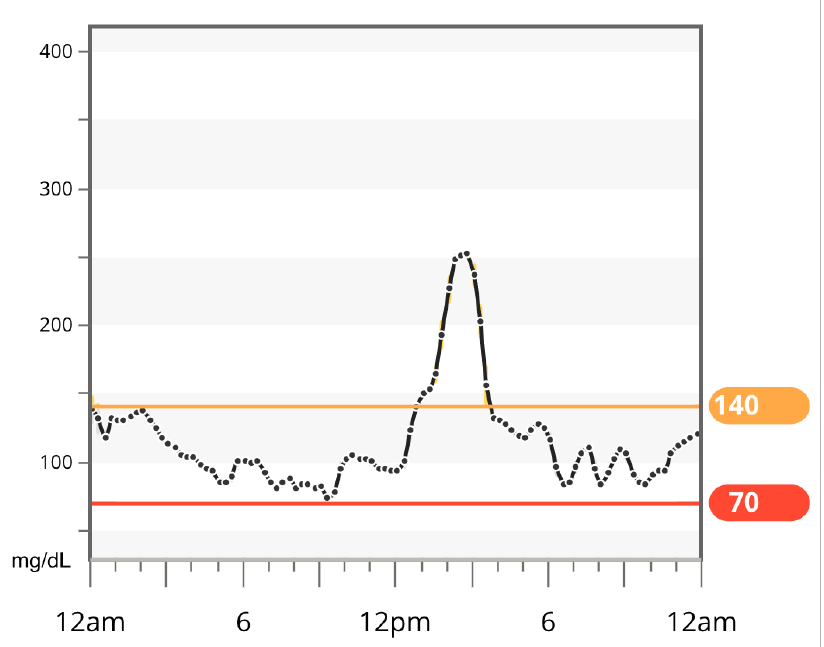
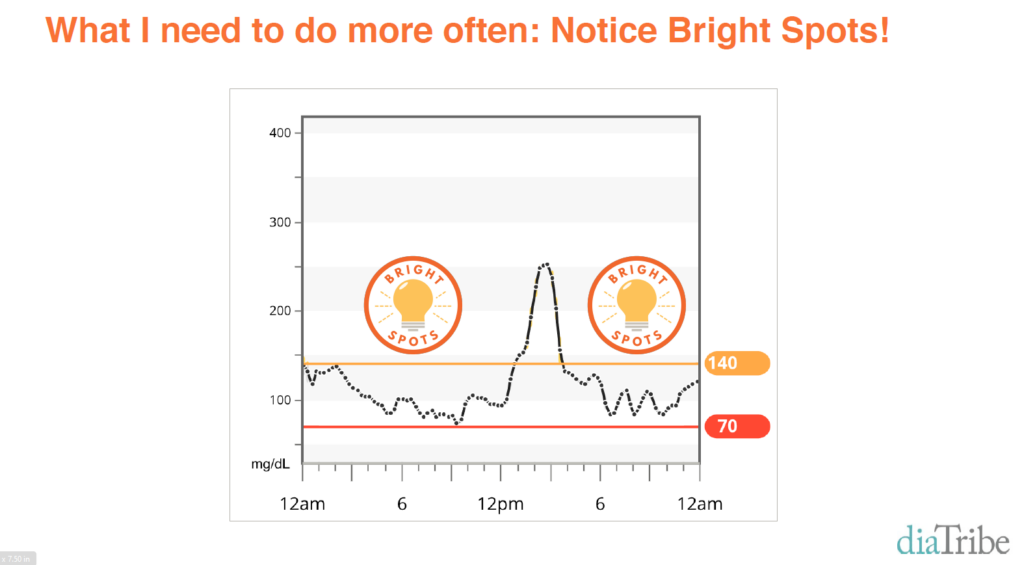
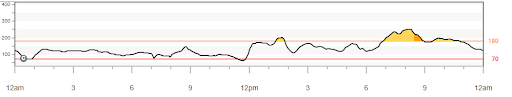
Evaluate what went well. After each event, reflect on what went well and how you can repeat that at future gatherings. This is a helpful solution-focused strategy for anyone! Also think about what didn’t go as planned, and what changes can be made at future gatherings to keep blood glucose in range. You can read more in our blog post on Bright Spots and Landmines.
If you are a health care professional and interested in learning more about our solution-focused practice and approach, when you subscribe to our blog, we’ll send you in return a FREE resource of 10 Solution-Focused Questions to start a solution-focused discussion with your clients.
Follow us on Twitter @AFreshPOVforYou
Deb is employed by Dexcom, but her words and opinions in this blog are her own.
Tami is employed by the University of Kentucky HealthCare Barnstable Brown Diabetes Center, but her words and opinions in this blog are her own.