The language for solution development is different from that needed to describe a problem. Steve de Shazer, pioneer of solution-focused brief therapy
If you are just catching up on our thoughts around transforming primary care visits by incorporating solution-focused (SF) tools and techniques, check out our last post about the benefits of using a SF approach. This week in our series we are spotlighting the power of words – meaning the words that we choose in conversations and interactions with clients. As the authors of the transformative paper The Use of Language in Diabetes Care and Education (Diabetes Care 2017;40:1790–1799 | ) call out:
“Words are immediately shaped into meanings when people hear or read them, and those meanings can affect how a person views him or herself…Words have the power to “elevate or destroy”.”
Person-first, strengths-based language
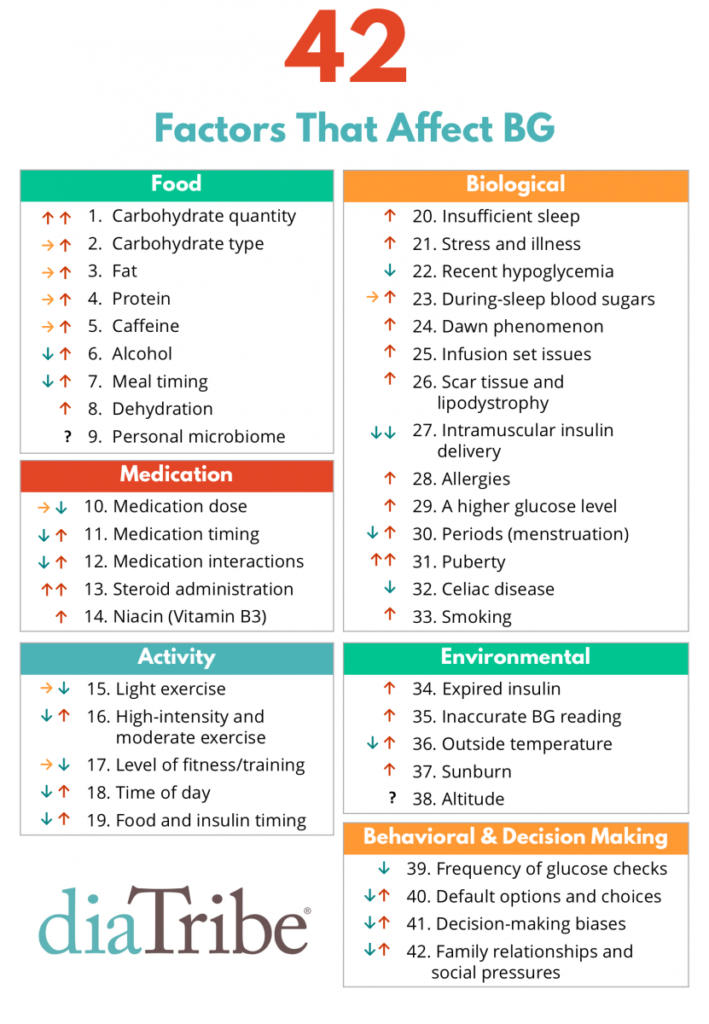
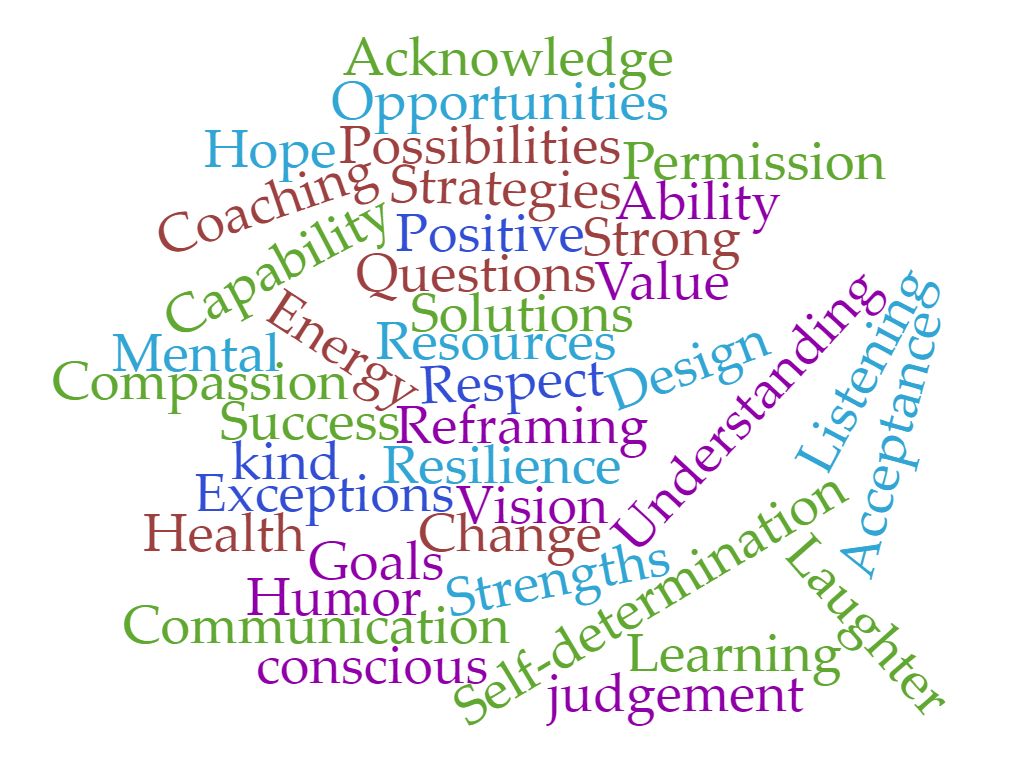
We’ve written extensively about the power and benefit of using person-first, strengths-based language in diabetes care and education and how #languagematters. Research clearly shows that positive language is associated with positive health outcomes. And on the flip side, when people are faced with language that is judgemental, blames and shames, they are less likely to share openly with their healthcare team.
3 examples of how flipping a few words can flip the conversation:
- Refer to one as a “person with diabetes”, rather than a “diabetic” (which labels them).
- Refer to “check” blood glucose, rather than “test” blood glucose” (which implies good/bad or pass/fail)
- Describe the scenario such as, “You take your medicine about half the time.”, rather than labeling one “noncompliant” (which shames)
A SF approach is not possible unless there is open communication facilitated by strengths-based language.
Why does language matter in primary care?
Again, language is powerful. We’ve discussed that the relationship between the healthcare provider (HCP) and the client is different. Instead of a hierarchical position, in SF relationships, the HCP and the client are considered “think partners”. They work together to identify solutions to move that individual forward towards achieving their goals. Thus, the language must follow to build the relationship.
Importantly, the goal for those with type 2 diabetes (T2D) is to feel they are part of a partnership in their diabetes management with their HCP, where they can discuss their challenges and their strengths and work together. Is it possible to create and strengthen this relationship when words such as non-compliant, cheating, not working hard enough, or other shaming and blaming words are used?
When we use words that focus on what people “can do”, and words that describe their actions, we recognize and acknowledge that diabetes is managed by the person living with it and we acknowledge that it’s one piece of their life and not their whole life. When a person living with diabetes engages with their primary care team as a partner, much can be accomplished. As we’ve noted before, you are able to “flip” the conversation from a negative to a positive and foster that “think partner” relationship.
Imagine a situation where an individual living with T2D looks forward to their primary care appointments because they are going to share with and learn from their HCP with no fear of judgment. They’ll talk about their struggles and challenges in a truthful manner and together they’ll identify areas that are working and small steps that can be taken to lead towards success.
The most important lesson you can take away from this discussion is that using strengths-based language is actually easy to do. As our friend and colleague Jane K. Dickinson says, “when you put the person first (not the diabetes), the language will follow.”
Our goal is that people living with T2D will develop a positive relationship with their primary care team, and all involved will understand the challenges, the opportunities, and the need for an empowering approach towards diabetes care and education. And we believe that a change in language can lead that.
If you’re not sure how to begin, consider starting your next encounter with one of these questions:
- Thanks for coming in today. What’s been going well for you in your diabetes management?
- It’s so nice to see you today, managing diabetes is really hard work – it’s like a part-time job. Tell me what you’ve been happy/pleased with about your diabetes management since we last met?
- We all need support in some manner. Diabetes is a team effort. How can I support you and support the changes you want to make? I’m here for you.
We hope you’ve been learning little nuggets with each blog post as you build your solution-focused tool box for managing T2D in primary care. Keep reading our series on incorporating a solution-focused approach when managing T2D in the primary care setting. Our goal is to start slow and share small, achievable, bite-size practice changes you can implement over time.
We welcome anyone interested in our approach to Subscribe to our blog and we’ll email you when a new post is published!
If you are a health care professional and interested in learning more about our solution-focused practice and approach, when you subscribe to our blog, we’ll send you in return a FREE resource of 10 Solution-Focused Questions to start a solution-focused discussion with your clients.
Follow us on Twitter and Instagram @AFreshPOVforYou
Deb is employed by Dexcom, but her words and opinions in this blog are her own.
Tami is employed by the University of Kentucky HealthCare Barnstable Brown Diabetes Center, but her words and opinions in this blog are her own.