“Dance like there’s nobody watching, love like you’ll never be hurt, sing like there’s nobody listening, and live like it’s heaven on earth.” ~ William Purkey
In our last post we celebrated that we only had three letters left in the alphabet to complete our A to Z series on solution-focused words to live by and use in practice. After sharing about the “unbothered” mindset for the letter U, we are now down to two letters, X and Z. Today is the letter X, and exploring the “ X-Factor”.
What is the X-Factor?
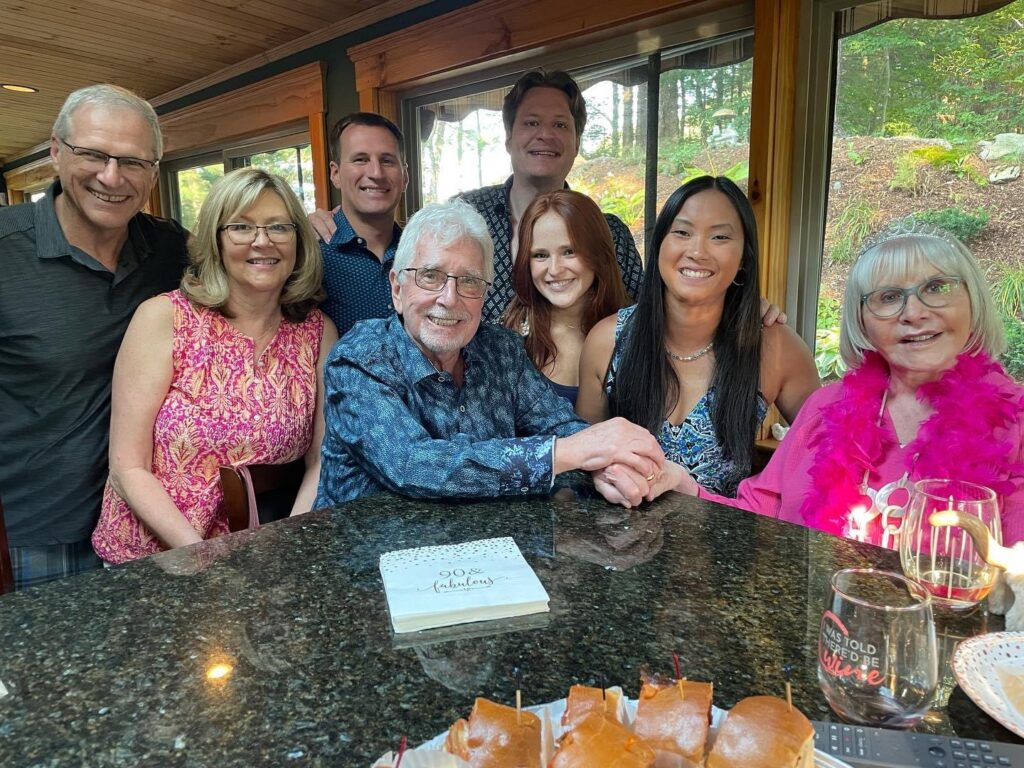
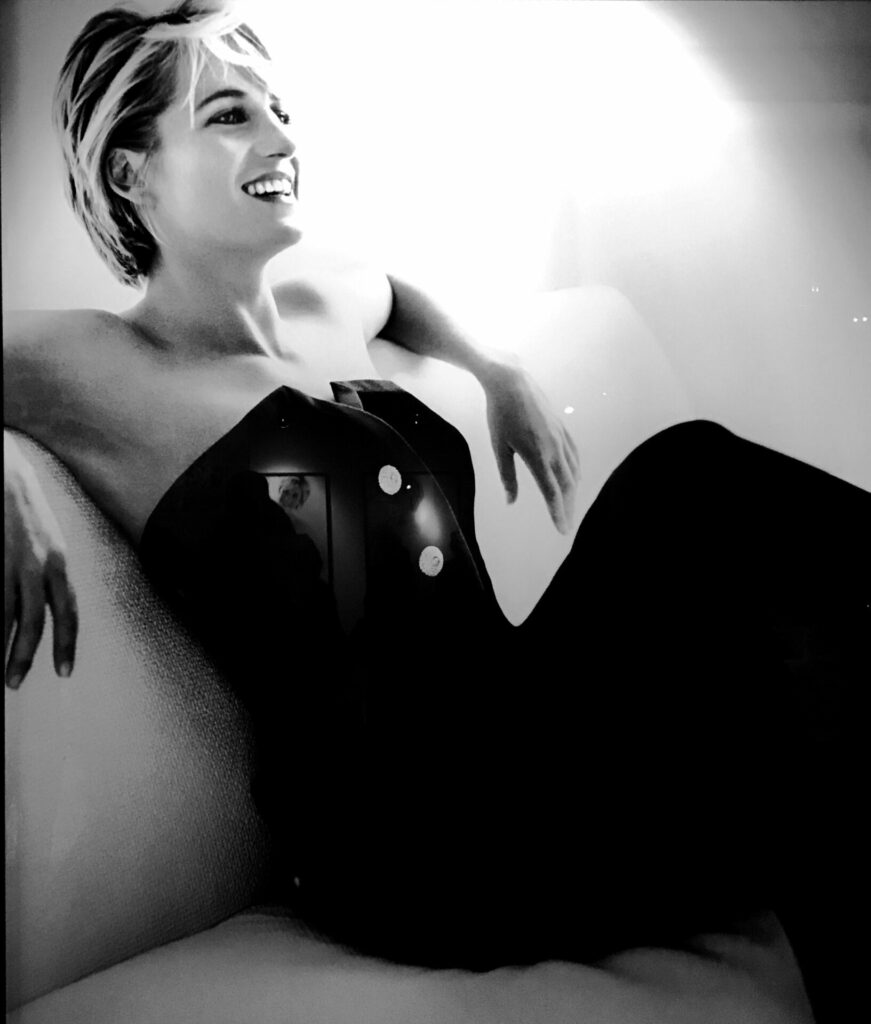
Have you ever met someone that was so easy to talk to, was truly engaged and interested in you and your discussion, and just genuinely enjoyable to be around? You might say they had a charismatic personality. They are someone you will remember, someone you’d like to spend more time with. Their magnetism may motivate, inspire optimism and hope, and move those around them. They have something that may be hard to describe. They just have “it”…..that “it” is the X-Factor. Princess Diana, pictured above definitely had the X-Factor. And we have several Diabetes Care & Education Specialist colleagues that immediately come to mind when we think of the X-Factor!
While brushing up on the X-Factor we identified some similarities to solution-focused tenets and practices we’ve written about before.
3 areas where we see overlap with an X-Factor personality and solution-focused life/practice:
- See “challenges” instead of “problems”.
A key element of a solution-focused life is focusing on Solutions instead of problems. Individuals who have the X-Factor embrace this thinking, and instead of seeing “problems” before them, they see “challenges”. They strive to make the best of what is in front of them and not waste energy on things they have no control over. They can see the world through a different lens and create a Fresh Point of View. If the world seems to have turned upside down, they see an opportunity to change their view, be grateful for the view, and come out on the other side with new solutions. This frame of thinking can be empowering to those around them.
- Focus on what’s important.
Those with the X-Factor personality fully embrace NOW. They see the present for what it is. They are able to break big challenges into smaller, digestible steps with focus on the here and now, and what’s important. They leave tomorrow’s challenges to another day.
As we’ve written about before, one way to focus on the important aspects of life is to use Reframing. Reframing is a simple and impactful tool that brings looking at a challenge from different angles, reimagining the situation, and identifying potential solutions. It helps identify “exceptions” (times when things were going well), so one can “do more of that”, instead of focusing on what’s wrong or not working. VIPs (the very important people in life) can be helpful in identifying opportunities for reframing as they know the individual and their habits well.
Another tool to keep focus on what’s important, is “imprinting”. We shared how to imprint in 5 easy steps here. When life is challenging (or just downright hard and painful), turning thoughts back to happy moments and picturesque views is a powerful reminder in the present.
- Embrace who you are.
An important characteristic of the X-Factor personality is embracing who you are. Having self-confidence and not caring so much what others think, or desiring their approval. Focusing on strengths, and maybe even embracing humor to not take oneself too seriously.
We hope that our readers now know that when they encounter someone with “it”, they have met an X-Factor! Embrace that X-Factor, learn from them, and appreciate how you feel when you’re around them.
We welcome anyone interested in our approach to Subscribe to our blog and we’ll email you when a new post is published!
If you are a health care professional and interested in learning more about our solution-focused practice and approach, when you subscribe to our blog, we’ll send you in return a FREE resource of 10 Solution-Focused Questions to start a solution-focused discussion with your clients.
Follow us on Twitter @AFreshPOVforYou
Deb is employed by Dexcom, but her words and opinions in this blog are her own.
Tami is employed by the University of Kentucky HealthCare Barnstable Brown Diabetes Center, but her words and opinions in this blog are her own.