Where you stand determines what you see and what you do not see; it determines also the angle you see it from; a change in where you stand changes everything. – Steve de Shazer, pioneer of solution-focused brief therapy
As we continue our series on transforming primary care encounters, today we’re tackling the topic of combatting therapeutic inertia.
What is therapeutic inertia?
In a general sense, “therapeutic inertia” is a lack of timely adjustment to the treatment plan when a client’s treatment goals are not being met. In the diabetes management arena, therapeutic inertia means being slow to add or change the care plan if a client’s A1C is above target. Delays in implementing the most effective care for each person with diabetes can happen at any phase of diabetes treatment and can range for instance from referring for diabetes and nutrition education, to starting the first medication, or intensifying medication management, including starting insulin.
Why stop therapeutic inertia?
The evidence is clear on two things:
- Managing glucose levels early in the course of diabetes leads to better long-term outcomes and reduces risk of complications.
- Those who reach their A1C targets soon after they’re diagnosed with diabetes are more likely to keep their glucose in target.
This is such a timely and impactful topic that ADA has launched an initiative called Overcoming Therapeutic Inertia. There are many resources for primary care clinicians to learn practical tips to focus on diabetes care in a proactive, timely way to improve outcomes. Learn more here.
Does shared decision making play a role?
One key tenet of shared-decision making is that all care decisions are discussed together with the client, and decisions are made together, which will ultimately mean more people with diabetes are following their treatment plan. Research shows us that when people are not involved in their diabetes medication decisions, they often no longer take the medicine.
When we talk about therapeutic inertia we are addressing both the clinician reluctance to advance therapy and the client’s reluctance to follow through with prescribed therapy. When we add shared decision-making we remove some of the barriers to medication taking. We discuss the potential side effects of the medication, costs, schedule and impact to their lifestyle. These are important decisions that need to be understood for individuals to embrace new therapy.
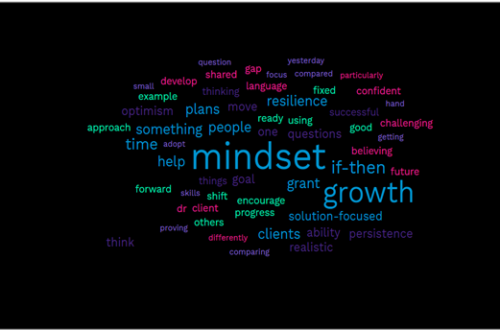
So how does incorporating a solution-focused approach address therapeutic inertia?
A solution-focused approach that encourages shared decision-making can be a tool to overcome inertia. As we’ve discussed previously, incorporating a solution-focused approach removes the shame and blame often associated with diabetes. When you discuss the clients goals and outcomes and what is working well for them, together you can identify the best therapy.
A solution-focused approach is a questioning approach, asking questions allows you to delve down to identify what is most important. An example of a medication-related question might be: What is most important to you when choosing a medication, the potential of weight gain or the need to check glucose before meals? ”And what else?” questions can be incorporated to learn more.
Since asking eliciting questions is a primary tenet, we encourage you to start all visits by listening and learning from your client. Remember, the client is the expert (read more about experts here), and even though they may be new to diabetes, they know what works in their life in other aspects, they know what they are capable of doing now.
When incorporating a solution-focused approach, each person will map out their own successful plan based on their lives, needs, strengths and desires. The care plan becomes personalized and directly relevant to the client. If something works, do more of it, help them recognize their strengths by identifying exceptions ( written about exceptions here.)
This solution-focused shared decision-making can build relationships and guide clients towards achieving goals, thus overcoming therapeutic inertia.
Next up
Join us next time as we continue our series on incorporating a solution-focused approach when managing T2D in the primary care setting. We’ll visit the moment of diagnosis with diabetes and share tips/tactics you can use to continue to help you build your solution-focused tool-kit.
We welcome anyone interested in our approach to Subscribe to our blog and we’ll email you when a new post is published!
If you are a health care professional and interested in learning more about our solution-focused practice and approach, when you subscribe to our blog, we’ll send you in return a FREE resource of 10 Solution-Focused Questions to start a solution-focused discussion with your clients.
Follow us on Twitter and Instagram @AFreshPOVforYou
Deb is employed by Dexcom, but her words and opinions in this blog are her own.
Tami is employed by the University of Kentucky HealthCare Barnstable Brown DIabetes Center, but her words and opinions in this blog are her own.