You can’t change your past. But you can let go and start your future.
– Quinn Fabray from Glee
Welcome to our new series, “Foster a Happy, Healthy Life” as we explore some simple yet powerful solution-focused tenets that you can share with patients/clients to fill their tanks and take care of themselves, as well as maybe incorporate in your own life. Trust us, you won’t want to miss out on this series!
It all starts with resilience
We’re kicking off with “It all starts with resilience”. We think about resilience as the ability to “bounce back” after challenging times. It’s having inner strength when life throws you challenges and still being able to hold your head up. Resilience is one of the skills essential for people with diabetes to develop in order to live well with diabetes. And yes, resilience is a skill. Research shows that resilience is a skill that can be developed over time with practice and support.
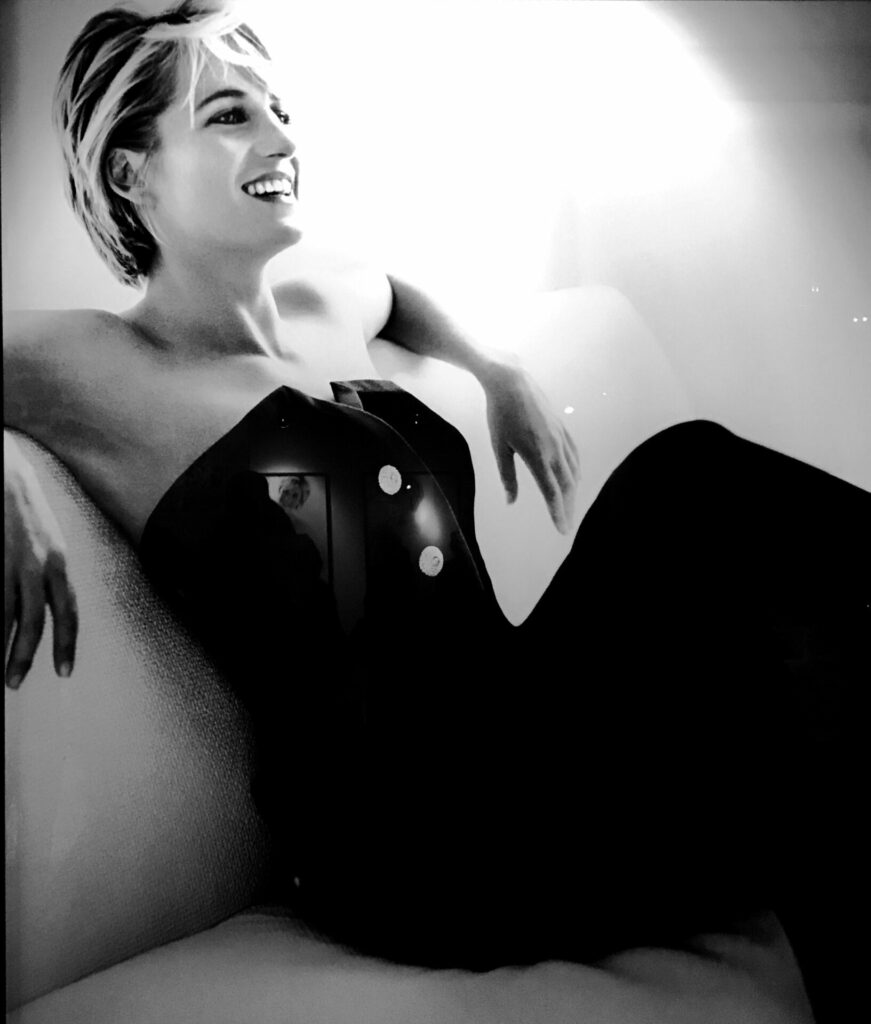
When we think of resilience and put a face to the word, one person that immediately comes to mind is Simone Biles. Just four years ago she dropped out of the Olympic games due to both physical and emotional challenges. And now here she is, back competing in the Olympics in a little over a week, defying odds. What inspiring resilience she demonstrates!
Having emotional agility can help navigate the twists and turns that diabetes – and life in general – throws out. We shared some about resilience in our Be REAL series here. Cultivating resilience can give the body and brain a boost when needed most!
Today we share 6 ways to boost resilience and strengthen your personalized resilience tool kit.
- Take on a challenge (even if it seems daunting) and step outside your comfort zone. Succeeding builds confidence and resilience.
- Find solutions, not excuses.
- Ask for support – it doesn’t mean you’re weak.
- Have an attitude of gratitude. We wrote about 3 great gratitude apps here that you may want to check out.
- Be intentional about taking care of yourself. (As Simone did when she withdrew from the 2020 Olympics).
- Find purpose in what you do each day.
What Simone (and other Olympic athletes along the way) have shown is the power of resilience! Without a doubt we’ll be tuning in to watch the gymnastics and cheer for Simone!
We welcome anyone interested in our approach to Subscribe to our blog and we’ll email you when a new post is published!
If you are a health care professional and interested in learning more about our solution-focused practice and approach, when you subscribe to our blog, we’ll send you in return a FREE resource of 10 Solution-Focused Questions to start a solution-focused discussion with your clients.
Follow us on Twitter @AFreshPOVforYou
Deb is employed by Dexcom, but her words and opinions in this blog are her own.
Tami is employed by the University of Kentucky HealthCare Barnstable Brown Diabetes Center, but her words and opinions in this blog are her own.