“Don’t ever diminish the power of words. Words move hearts and hearts move limbs.”
-Hamza Yusuf
In our last post we began a 4-blog series called, “Be REAL”, revisiting some powerful words that can advance a solution-focused practice. The 4 words we’ll focus on make up the acronym REAL:
- Resilience
- Experts
- Acceptance and
- Listening
You can catch up on our last post on Resilience, the R in REAL on October 25, 2023.
Today’s word is EXPERTS
According to Dictionary.com, an “expert” is a person who has a special skill or knowledge in some particular field.
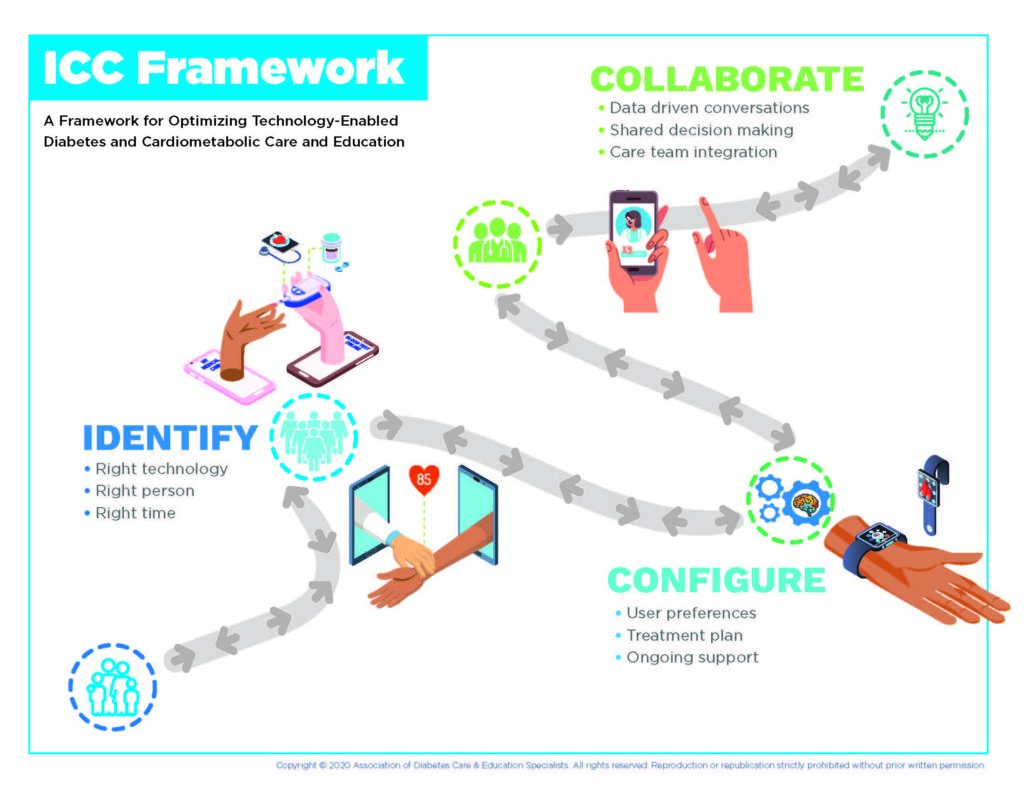
So in the world of diabetes care and education, a diabetes care and education specialist (DCES) may first come to mind as the “expert”. Yet, we challenge you to think beyond that. Have you heard the term “expert patient”? That refers to the inherent knowledge that individuals living with diabetes (or other chronic conditions) have about their condition, its impact on their life, and what decisions they feel comfortable making. People with diabetes (PWD) are the true experts in their lived experience with diabetes.
That said, just because one has a chronic condition does not imply that they have expertise in dealing with it. That presents the opportunity for the DCES to step alongside the PWD as a “think partner”. In a solution-focused interaction, the relationship between the healthcare provider and the patient/client is different. Instead of a hierarchical position, in solution-focused relationships, the DCES and the patient/client are considered “think partners”. They work together to identify solutions to move that individual forward towards achieving their goals. The DCES helps develop solutions by asking their patient/client questions and helping them to use their own personal strengths to create solutions that work for them.
Be a think partner: 7 questions to try
- What do you know about yourself that lets you know you can achieve what you want?
- What would success look like for you (e.g. in life, in living with diabetes etc.)?
- What strengths do you have and use to help you manage your diabetes every day?
- How can you use your strengths to create opportunities for success?
- What is one thing you have come to accept in your life that took some time to process?
- How did you feel when you were finally able to accept that challenging situation?
- How could you use those experiences and feelings to move you forward to accept a new challenge now?
For more on EXPERTS, here is our first blog we wrote on EXPERTS back in 2020: Experts
Join us next week as we focus on the A in Be REAL: Acceptance!
We welcome anyone interested in our approach to Subscribe to our blog and we’ll email you when a new post is published!
If you are a health care professional and interested in learning more about our solution-focused practice and approach, when you subscribe to our blog, we’ll send you in return a FREE resource of 10 Solution-Focused Questions to start a solution-focused discussion with your clients.
Follow us on Twitter @AFreshPOVforYou
Deb is employed by Dexcom, but her words and opinions in this blog are her own.
Tami is employed by the University of Kentucky HealthCare Barnstable Brown Diabetes Center, but her words and opinions in this blog are her own.