Problem talk creates problems. Solution talk creates solutions. – Steve de Shazer, pioneer of solution-focused brief therapy
Managing diabetes is complex. We know that. Constant focus on “problems” can erode confidence. So, clients may turn to us, their healthcare team, looking for guidance to do something different.
As we continue our new series on transforming primary care encounters by using a solution-focused approach, today let’s talk about WHY use this approach. We’ve had several primary care providers encourage us to share more on this approach as they found it to be a transformational way of thinking and engaging with clients. So let’s delve a little deeper today…this is one way of thinking that may help.
Before we begin, one significant difference in a solution-focused approach is use of the term “client” instead of “patient.” In a solution-focused approach the clinician and person with diabetes are considered “think partners” working together to manage diabetes. Thus, the term client is more inclusive and more indicative of the approach, and is what we use. (That said, we realize that the term “patient” is widely used in many healthcare settings and we respect that.)
Why use a solution-focused approach in primary care?
Since the majority of type 2 diabetes (T2D) is managed in primary care, it seems that the best place to start to change the way we engage with clients is through primary care. Without a doubt there are many competing demands during a primary care visit. And visits can often focus on “fixing” “problems” as the limited appointment time flies by.
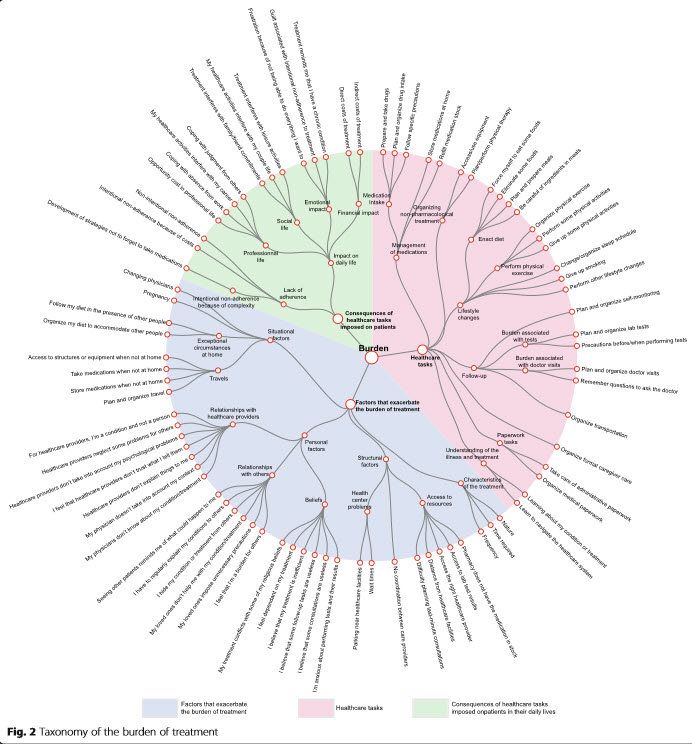
The Taxonomy of Burden of Treatment, published in 2015, identifies three areas where people with chronic conditions, such as diabetes, have “work to do”. So, if a person does “everything” the guidelines ask them to do, that would take about 2.5 hours/day… that’s like a part-time job – a job they didn’t ask for! And those 2.5 hours don’t take into account the nuances of the impact on their life, and factors that make living with chronic conditions challenging, like work, travel, lack of income etc.The constant focus on problems can make living with T2D even harder.
Considering the complexity of chronic care can help build compassion and recognize the reality of day to day life – what we’re asking people to do – and how it is impacting everything else. The way a person is treated and the way they feel about living with diabetes impacts outcomes. When doing all this work to manage their diabetes and then see their care team focus on what’s wrong or what’s not happened, instead of what is working well, negates all their hard work. This is where language and communication are key.
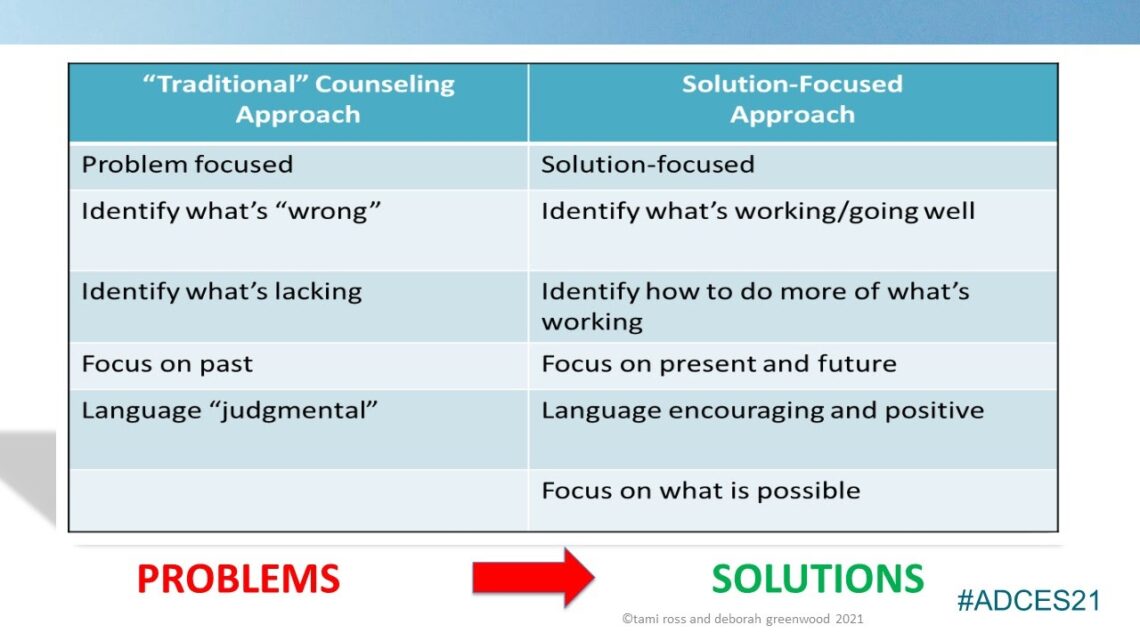
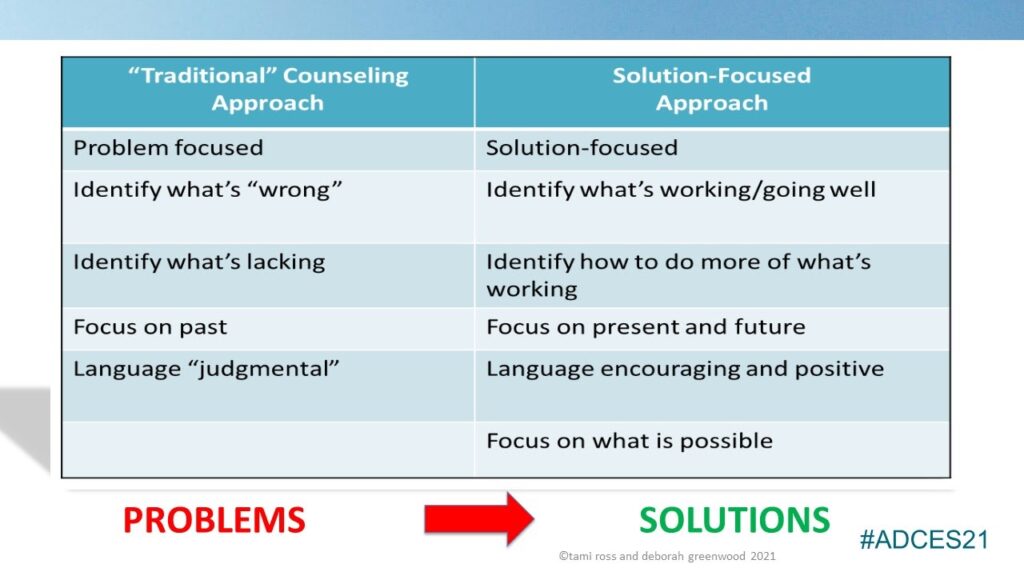
In the image at the top of this blog you can see a quick summary of how the interaction can be “flipped”. Incorporating a solution-focused approach can enhance your client relationships and build trust and open communication needed for successful diabetes management.
Join us as our series continues on incorporating a solution-focused approach when managing T2D in the primary care setting. We’ll share how you can incorporate the tenets into a brief visit and how you can build your solution-focused tool-kit over time. Our goal is to start slow and share small, achievable, bite-size practice changes you can implement over time. Our next post will focus on benefits of this approach for the primary care team, both clinician and person with diabetes.
We welcome anyone interested in our approach to Subscribe to our blog and we’ll email you when a new post is published!
If you are a health care professional and interested in learning more about our solution-focused practice and approach, when you subscribe to our blog, we’ll send you in return a FREE resource of 10 Solution-Focused Questions to start a solution-focused discussion with your clients.
Follow us on Twitter and Instagram @AFreshPOVforYou
Deb is employed by Dexcom, but her words and opinions in this blog are her own.
Tami is employed by the University of Kentucky HealthCare Barnstable Brown DIabetes Center, but her words and opinions in this blog are her own.