“Wellness is the complete integration of body, mind and spirit – the realization that everything we do, think, feel and believe has an effect on our state of well-being.” ~ Greg Anderson

We’ve just returned from a relaxing vacation in the South of France where we imprinted enough “fresh views” to last us quite a while! But we are quickly back to work, with the first stop post vacation at The American Diabetes Association Scientific Sessions in San Francisco. A Fresh POV for You attended some inspiring sessions, particularly those focused around behavioral health. (If you’ve been following our blog, you know that’s a special interest of ours.) We thought we’d share highlights from several that were particularly impactful.
Highlight #1
One of the most rewarding presentations was the Richard R. Rubin Award lecture, presented by Dr. Frank J. Snoek, PhD. The award recognizes an individual who has contributed to the science of the behavioral aspects of living with diabetes. Dr. Snoek’s talk #DiabetesPsychologyMatters focused on the important connection between behavior change and mental health. As one of his slides depicted…they are two sides of the same coin!
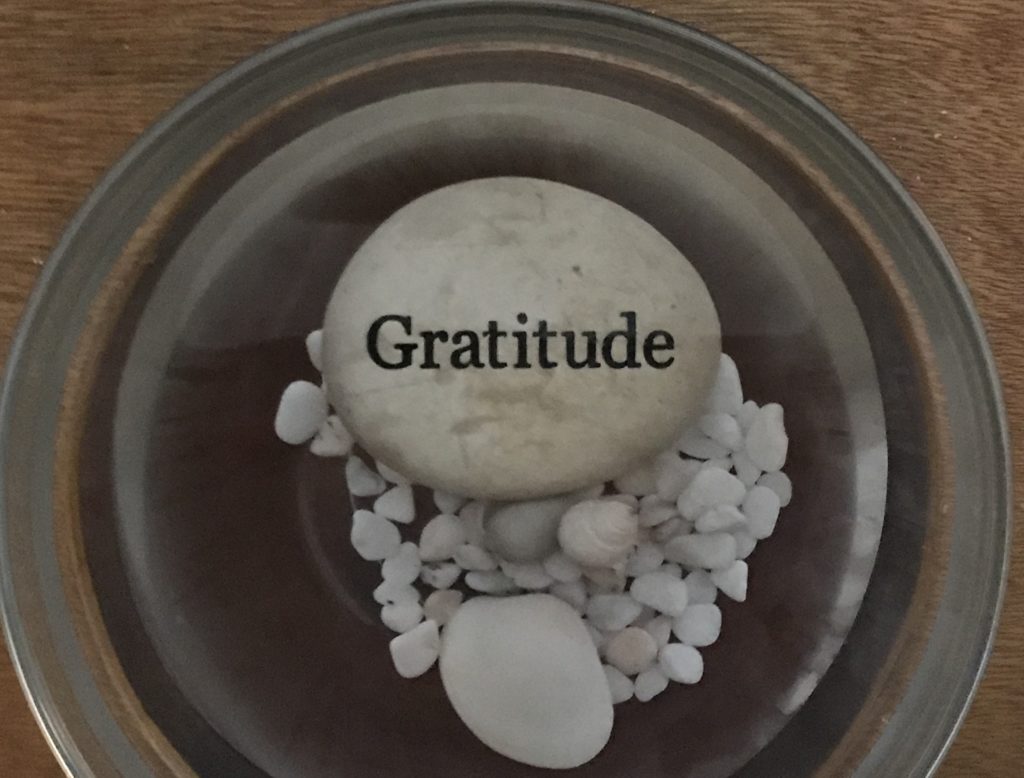
Dr. Snoek noted that one goal is to shift the burden of diabetes distress, so that higher distress can be moved down to moderate, and moderate moved down to low. He also indicated that a single high score on a distress scale does not mean that an individual needs professional help, or is in a maladaptive situation. Everyone with diabetes experiences diabetes distress at some point and at some level.
Additionally, he discussed the correlation between mood and behavior, an area of significant interest to us at A Fresh POV for You. He described that when someone actually feels good, they are able to shift their priorities towards less pleasant activities that might help them achieve more long term goals. However, when someone has a low mood, they tend to seek short term rewards to help them feel better in the present.
Overall he emphasized the need to enhance access to care and specifically called out what he described as “indirect interventions” – including Diabetes Self Management Education and Support (DSMES), psycho-education as well as internet/mobile interventions. Specifically, he called for incorporating behavioral techniques along with existing pure “education” practices.
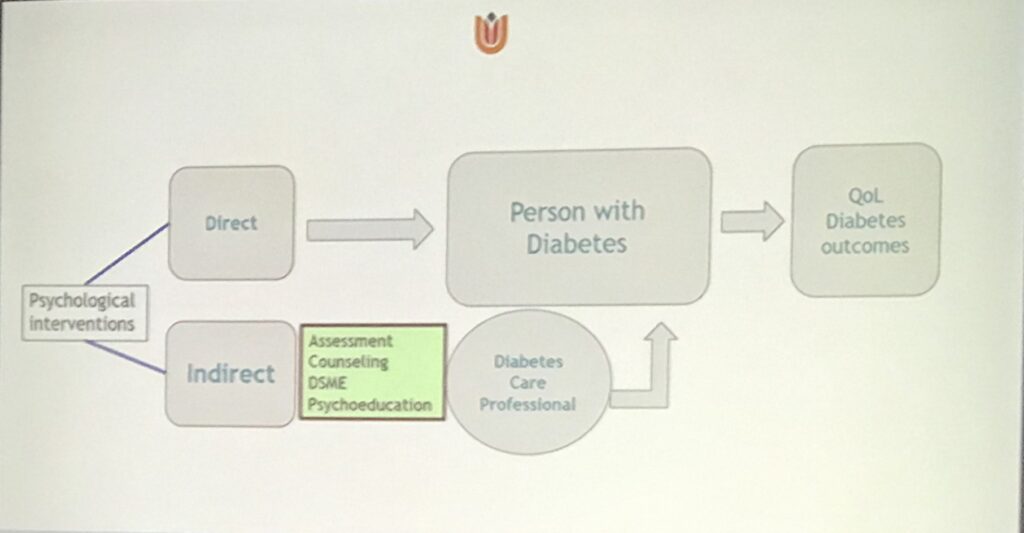
We believe that by incorporating Solution-Focused Brief Therapy (SFBT) techniques and counseling approaches, diabetes educators can address the needs of people living with diabetes, incorporating “two sides of the same coin”. Addressing both the self-management education and support needed for behavior change, while at the same time, addressing mental health concerns, such as diabetes distress. In essence, we can “fill the gap” that exists in access to psychological care. Overall this lecture solidified our efforts in moving this approach forward within the diabetes community.
Highlight #2
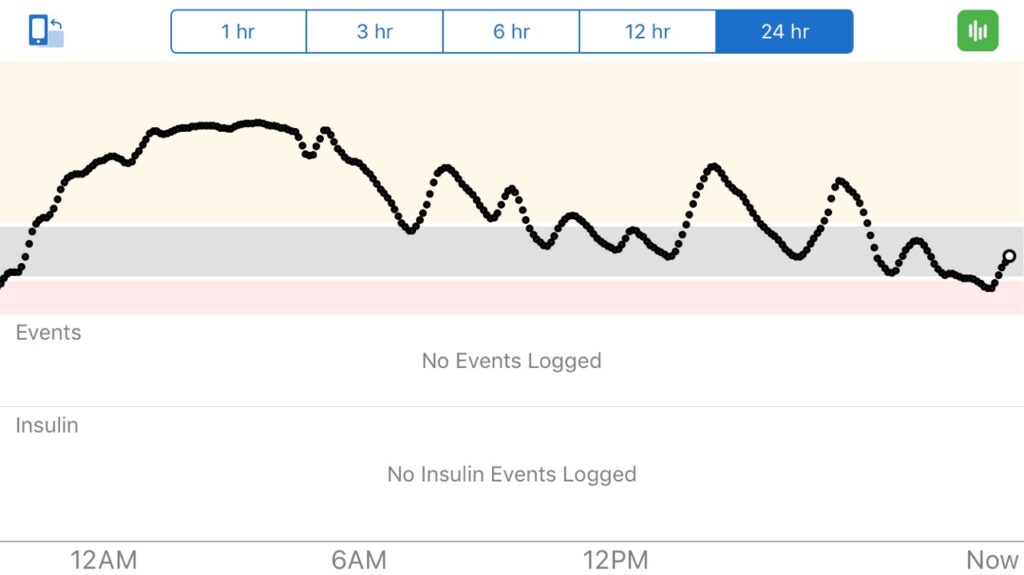
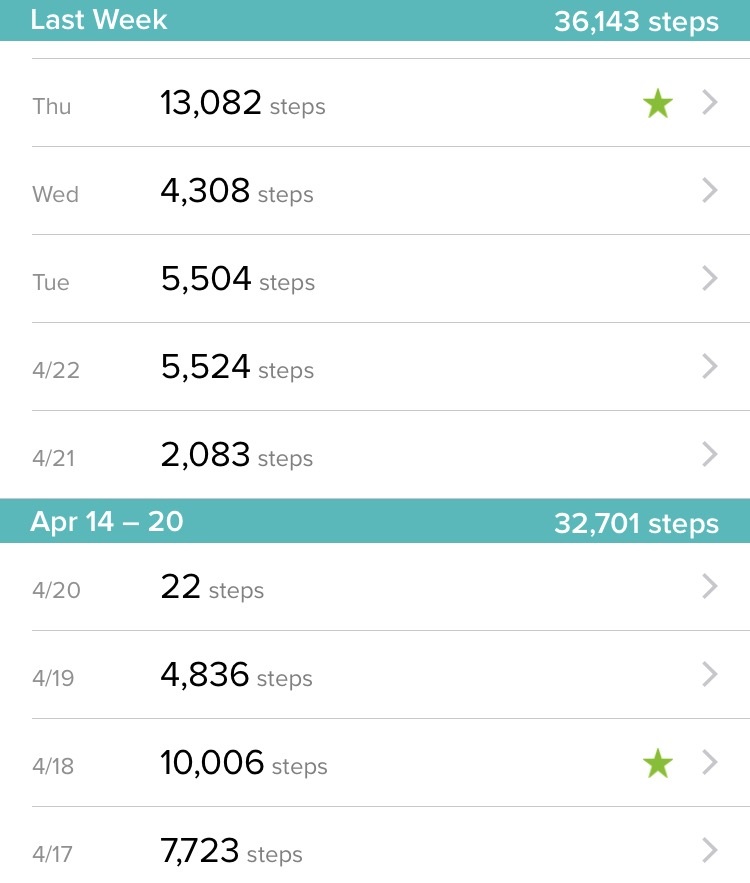
Another impactful session focused on complications associated with diabetes. The emotional toll of diabetes complications-What have we done for them lately. The panel was moderated by Dr. Korey Hood, a behavioral scientist. Panelists included Chris Aldred (aka The Grumpy Pumper), Kerri Sparling (Six Until Me), Matthew Heywood, and Ina Mendoza. They spoke frankly and candidly about their experiences living with diabetes complications. Managing diabetes is tiring enough, then add a complication, and it becomes so much more complex. Much of the discussion addressed the stigma associated with diabetes complications and how the panelists were/are often told that they “should have done better”. Ouch. #LanguageMatters when talking about complications. Making people often feel “less than” when they have a complication. Where is the compassion in care?
One question from the audience was, “What can we do to make this better?” So, A Fresh POV for You posed an answer to consider….”How about incorporating a more solution-focused approach into practice? With focus on the solutions and strengths an individual has to help move them forward, rather than focusing on past problems and trying to identify why they occurred.” We know that no matter how much effort goes into managing diabetes, sometimes people still get complications. We also referred to Adam Brown’s Book, Bright Spots and Landmines,, featured in one of our April blog posts. Focusing on “bright spots” are similar to focusing on the “exceptions” or the things that are going well used in a solution-focused approach.
We look forward to sharing more of these concepts in our presentation at the American Diabetes Association Annual Meeting in Houston in August, Applying the Miracle Question in Diabetes Care.. In fact, here we are finalizing our slides before the deadline while in Marseilles, France.

Highlight #3
Stigma was a theme common through many of the behavioral health sessions. As recipient of the Outstanding Educator in Diabetes Award, Virginia Valentine, shared a moving presentation, The most important thing we give to people is…Hope: Overcoming stigma in diabetes and obesity,. She explained that the stigma associated with diabetes causes blame and shame, and that “Shame is the intensely painful feeling or experience of believing that we are flawed and therefore unworthy of being loved or belonging.”-Brene Brown. She reminded the audience that “the only thing people with diabetes did wrong is when they picked their grandparents.” She ended her presentation with a review of the language guidelines that foster person-first, strength based language.
Highlight #4
Finally, there was the session on #LanguageMatters- Strategies to Improve Communications in Diabetes Care. Jane K Dickinson, and Joe Solowiejczyk, both healthcare providers and people living with diabetes, gave their perspectives on the use of language. Notably, Jane was the lead author on the publication , The Use of Language in Diabetes Care and Education (we’ve written about #languageMatters in the past here). Then Kevin Joiner connected the dots between the stigma associated with language when engaging in a healthcare discussion. Finally, Dr. Jane Speight, lead author of the Australian Position Paper, A New Language for Diabetes, helped to identify strategies for healthcare providers to communicate more effectively with people living with diabetes. We were excited to see them show the Telly Award Winning #LanguageMatters video that was co-designed with the #DOC and released last year at the AADE meeting, Changing the Conversation.

Check back July 10th as we share another big highlight from ADA Scientific Sessions, discussion of the recently published “Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report”.
Subscribe to our blog and we’ll email you when a new post is published!
Follow us on Twitter and Instagram @AFreshPOVforYou.