“I realized that my sugar was like a rollercoaster. It would go up and down very clearly. So I started to go for walks. Not light walks, but fast-paced ones.” ~Study participant
Since the COVID-19 pandemic began the disparities in diabetes technology use in underserved populations has risen to the forefront. During the recent American Diabetes Association (ADA) Scientific Sessions data were shared about a novel use of an online peer support community combined with continuous glucose monitoring (CGM) use to educate, engage and empower people with type 2 diabetes. Since Deb was a co-investigator on this study, we reached out to Dr. Michelle Litchman, PI, Assistant Professor, University of Utah, College of Nursing to discuss the study findings and impact.
The ADA abstract: 151-O Using a CGM plus Online Peer Support Community Intervention to Address Health Disparities
Dr. Litchman, what makes this study unique and important?
This study was developed based on two separate PCORI-funded projects that incorporated community-based participatory research principles and community advisory boards (CAB). The first CAB partnered with individuals within the Hispanic community to better understand diabetes technology needs and desires. The second CAB included diabetes online community partners to best understand how online peer support could reinforce diabetes technology use and healthy behaviors.
What were the components of the study?
We developed an intervention that combined continuous glucose monitoring (CGM) plus an online peer support community (OPSC). To support the needs of Hispanic and Spanish-speaking adults with type 2 diabetes not using insulin, the CGM+OPSC intervention was optimized to be culturally and linguistically appropriate. Participants wore CGM to visualize their daily glucose patterns and engaged in weekly personal experiments. Personal experiments included health behavior challenges related to general diabetes topics (being active, healthy eating, etc.) and were posted to the OPSC weekly. The OPSC were managed by trained Spanish/English bilingual peer facilitators who also lived with diabetes and used CGM. This mixed method study assessed how participants used the intervention.
Participants completed a 1-week blinded baseline CGM recording (N=31) then engaged in the CGM+OPSC intervention for 12 weeks. Of those that continued into unblinded phase (n=22) study engagement was excellent (N=21).
What were some of the key outcomes of the study?
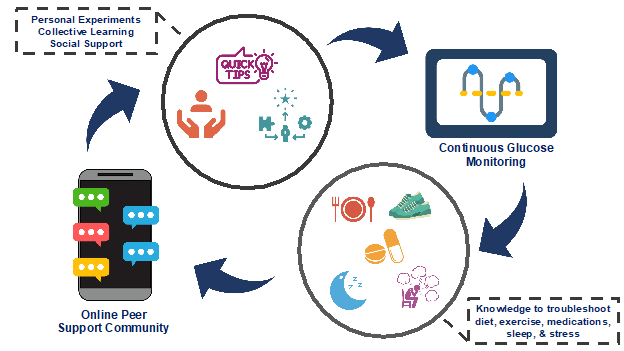
We analyzed exit interviews and identified 3 themes: (1) CGM “personal experiments” helped participants gain knowledge about how diet, exercise, medications, stress, and sleep impacted glucose levels; (2) the OPSC reinforced healthy behaviors through personal experiments, collective learning and social support; and (3) CGM engagement increased OPSC participation and participation in the OPSC resulted in greater CGM utilization, suggesting a positive feedback loop.
We also found that self-efficacy levels significantly improved when comparing pre to post intervention.
Tell us about the figure you presented.
The figure above describes a positive feedback loop in which CGM could help see how glucose levels changed when they engaged in health behaviors, and the OPSC provided structure (personal experiments) and emotional and informational support to reinforce healthy behaviors. The promise of diabetes technology can only be seen with continued use. This study showed that an OPSC is one way to enhance CGM use. It is possible that OPSC could support other diabetes technologies and in other populations or languages.
Tell us more about the peer facilitators.
We hired and trained five Hispanic Spanish/English bilingual individuals who were living with diabetes and using CGM. Having a group of peers that the participants could relate to was critical to the study’s success. The peer facilitators could provide tips and tricks from their own lived experience while also providing encouragement to those who might be struggling. All peer facilitators were supported by the research team and a bilingual certified diabetes care and education specialist. After the study completed, the peer facilitators helped develop training videos to support future research.
What is the key message you would like readers to take away today?
Hispanic, Spanish-speaking adults with type 2 diabetes have a great desire to use diabetes technology. However, diabetes technology must be optimized for language, cultural and social support needs. The CGM+OPSC intervention provided participants with the tools necessary to learn, problem-solve, and make healthy behavior changes and is a promising intervention to address health disparities.
Is there anything else you would like us to know?
This study would not have been possible without important community partners. We thank the CABs from both PCORI studies who helped guide us to developing this novel intervention.
Of note, this abstract was awarded “Best Abstract” in the Glucose Monitoring and Sensing presentation group! We congratulate and thank Dr. Litchman for sharing the ADA presentation with us and look forward to future publications.
Stop back by in 2 weeks to see what we write about as we continue to share about a variety of other technologies that impact and influence diabetes care and education!
We welcome anyone interested in our approach to Subscribe to our blog and we’ll email you when a new post is published!
If you are a health care professional and interested in learning more about our solution-focused practice and approach, when you subscribe to our blog, we’ll send you in return a FREE resource of 10 Solution-Focused Questions to start a solution-focused discussion with your clients.
Deb is employed by Dexcom, but her words and opinions in this blog are her own.
Tami is employed by the University of Kentucky HealthCare Barnstable Brown DIabetes Center, but her words and opinions in this blog are her own.